Wound debridement (pronounced duh – breed – muhnt) is the process of removing dead tissue from wounds. It is necessary for healing because dead tissue hinders the growth of new cells and makes it easier for infection.
Why does my wound need to be debrided?
- Dead tissue can trap bacteria, which can lead to a wound infection. Wounds can heal faster if the dead tissue is removed.
- New tissue is unable to grow with dead tissue on the wound.
- Dead tissue can hide pockets of pus. Pockets of pus can develop into an infection.
- Infection can prevent your wound from healing and can cause a life-threatening illness.
- Removing dead tissue regularly keeps it clean. It will help your wound grow new tissue, and the wound can heal faster.
- It is important that all dead tissue be removed. Sometimes, the wound may appear larger after debridement.
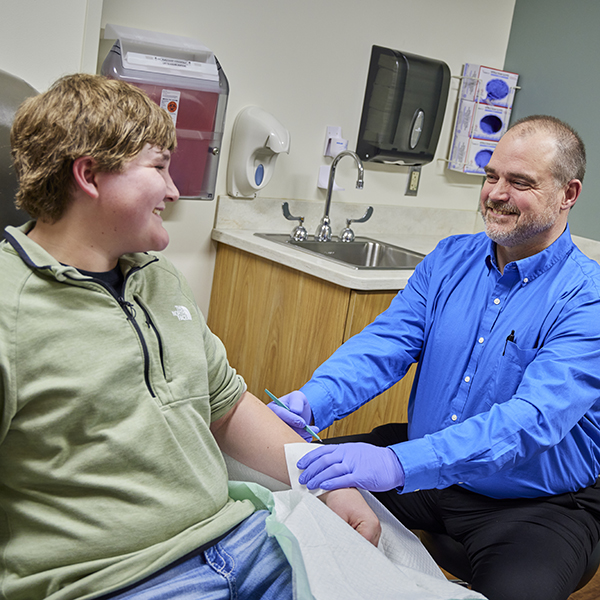
What can I expect during a wound debridement?
During a wound debridement, you can expect a hands-on procedure focused on removing dead, infected, or damaged tissue so your wound can heal properly. What you experience depends on the type of debridement and the condition of your wound.
Here’s a clear breakdown of what usually happens:
1. Arrival and Assessment
- A nurse or wound care specialist will check your wound: size, depth, color, drainage, odor, and signs of infection.
- They’ll review your medical history, medications, and pain levels.
- You may have photos or measurements taken to track healing.
2. Wound Cleaning
- The area around the wound is cleaned with saline or antiseptic.
- If there’s a dressing, it’s removed carefully.
- Local anesthesia (numbing gel or injection) may be used depending on the method and expected discomfort.
3. Debridement Procedure
This step varies by type of debridement:
| Type | What Happens | Pain Level |
| Surgical (sharp) | A provider uses scalpel, scissors, or curette to cut away dead tissue | Moderate (local anesthetic often used) |
| Mechanical | Gauze or special tools used to scrub or pull away tissue (e.g., wet-to-dry dressings) | Can be painful, especially if dry |
| Enzymatic | A prescription ointment is applied to soften and dissolve dead tissue | Minimal pain |
| Autolytic | A moist dressing helps your body’s enzymes break down tissue naturally | Painless |
| Biological (maggot therapy) | Sterile maggots are placed on the wound under a dressing to eat dead tissue | Mild tingling, rarely painful |
4. Dressing the Wound
- After debridement, your wound will be:
- Rinsed and cleaned again
- Dressed with antimicrobial, moisture-retaining, or absorbent materials
- You may receive foam, alginate, hydrogel, or other dressings based on wound typ
5. How to Care for a Wound after Debridement
You’ll be given:
- Instructions on how to care for your wound at home
- A schedule for follow-up visits or additional debridement
- Pain management advice, if needed
What You Might Feel:
- Pressure during the procedure
- Stinging or burning (especially during mechanical or sharp debridement)
- Soreness afterward, similar to a scraped knee or minor burn
- Discomfort during dressing changes if tissue sticks
Tips:
- Let the team know if you’re feeling too much pain — they can adjust
- Follow all home care instructions exactly to avoid infection
- Track changes: note pain, redness, swelling, discharge, or odor
FAQs
Does wound debridement hurt?
Wound debridement can cause some pain or discomfort, depending on the method used and the wound’s severity. Surgical and mechanical debridement are more likely to be painful, while enzymatic or autolytic debridement methods are generally gentler and less invasive. To ensure patient comfort, wound care specialists often use local anesthesia, numbing agents, or pain medication during the procedure. While some soreness may occur afterward, this discomfort is typically manageable and temporary. Effective pain control is a key part of professional wound care, and patients are encouraged to speak with their provider about pain management options before undergoing debridement.
How many times can you debride a wound?
There is no universal limit to how many times a wound can be debrided. Chronic or non-healing wounds, such as diabetic foot ulcers or pressure injuries, may require multiple debridement sessions over time to remove dead tissue and promote proper healing. The number of debridement procedures needed depends on the wound’s response to treatment, the presence of necrotic or infected tissue, and overall patient health. Regular wound assessment by a qualified wound care specialist ensures that debridement is performed as often as necessary to support optimal wound healing.
How often should you debride a wound?
Wound debridement should be done as often as needed to remove dead or infected tissue and promote healing, which varies based on the type and severity of the wound. In many cases, wounds are debrided weekly or biweekly, especially if they are slow to heal or show signs of infection. For chronic wounds, regular debridement is often essential to maintain a clean wound bed and enhance the effectiveness of other wound care treatments. A healthcare provider will create a customized wound care plan, including the appropriate frequency of debridement, to ensure the best possible healing outcomes.
When does a wound need to be debrided?
A wound typically needs to be debrided when there is dead, damaged, or infected tissue preventing the healing process. Common signs include black eschar, yellow slough, increased drainage, foul odor, or delayed wound healing. Debridement is an important step in advanced wound care, as it removes non-viable tissue, reduces the risk of infection, and prepares the wound for new tissue growth. Not all wounds require debridement, so a proper evaluation by a wound care professional is essential to determine whether this procedure is necessary for optimal recovery.
We’re here to help!
Our compassionate Wound Care Specialists at Glencoe Regional Health will take good care of you. To schedule an appointment, call 320-864-7040.