Symptoms of Lymphedema:
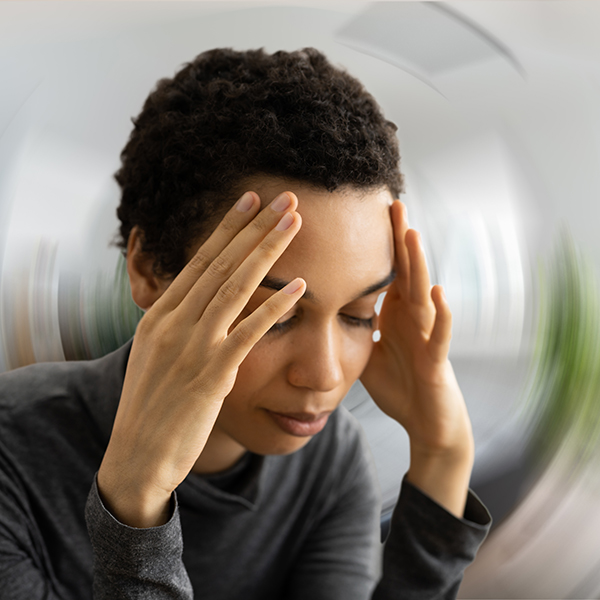
- Slow onset: you may not even notice the swelling in the early stages of lymphedema
- Progressive worsening of swelling over time
- Typically starts distally (from the bottom and goes up)
- Creates discomfort: your joints may feel tight or inflexible, parts of your body may feel heavy or full, and you may have a feeling of burning or itching
- Skin changes can occur, including your skin becoming thicker
Stages of Lymphedema:
Stage 0: The lymphatic system is compromised, but swelling is not yet present to touch or with measurements. The body part might feel heavy, achy, or full.
Stage 1: There may be occasional swelling that goes away, especially with elevation. The body part often feels heavy, achy, or full.
Stage 2: The affected area is almost always swollen, and your skin may feel firmer than the surrounding areas.
Stage 3: The affected area has significant swelling with changes in your skin such as changes in color and texture.
Who May Benefit from Lymphedema Therapy?
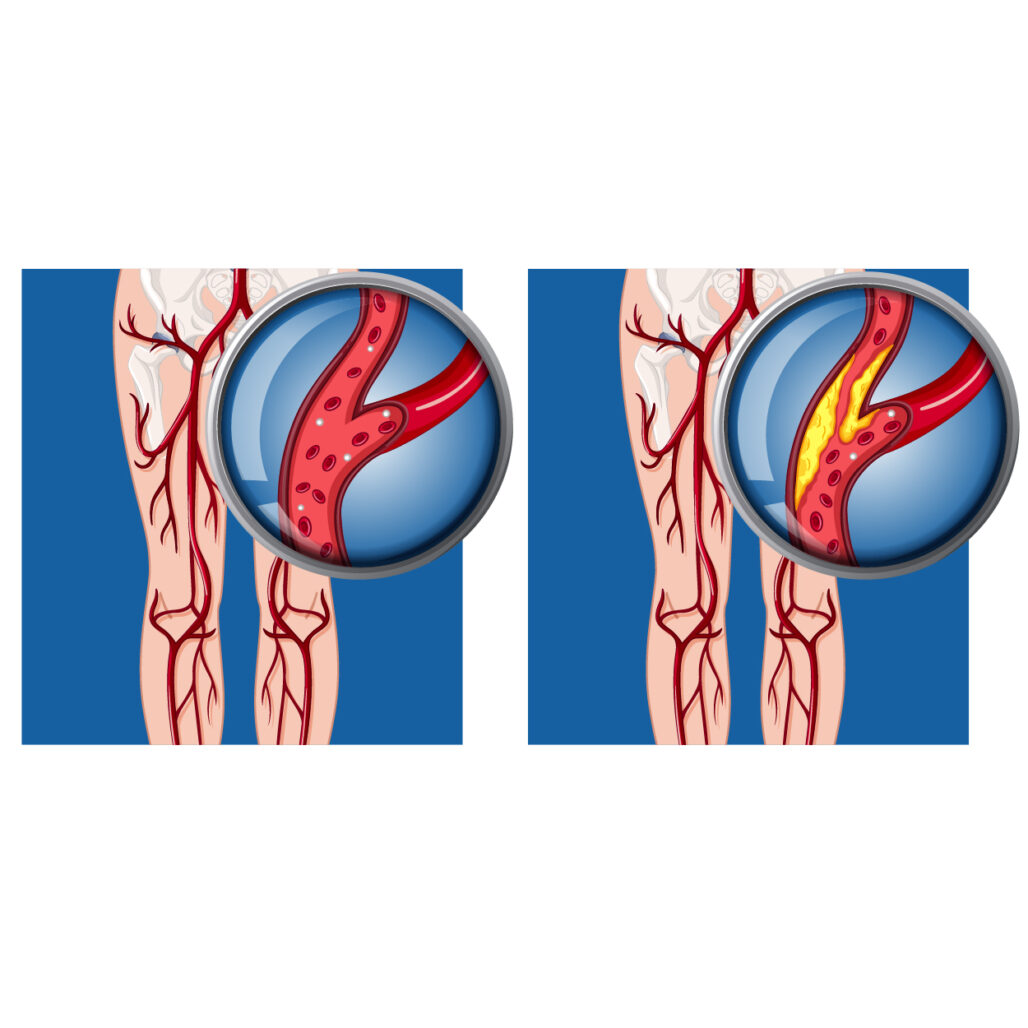
Patients who benefit from treatment include those with chronic venous insufficiency, primary lymphedema, and lymphedema secondary to cancer treatment. Orthopedic patients who do not progress as expected in edema reduction following surgery or injury are also candidates for treatment.
What is Lymphedema Therapy Treatment?
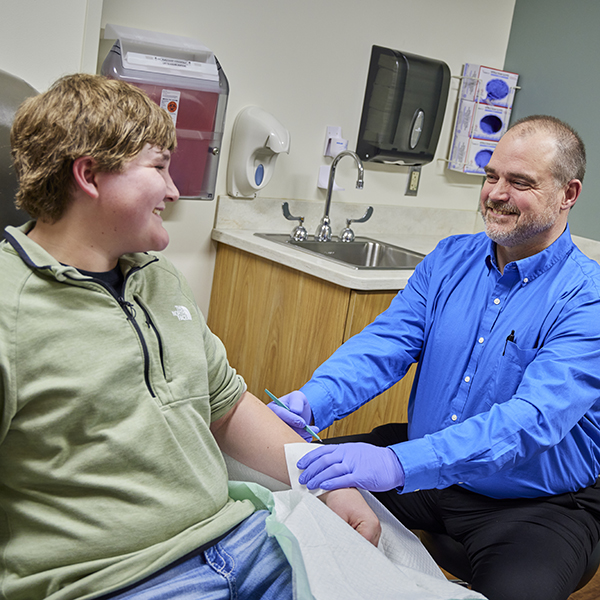
Complete decongestive therapy consists of manual lymph drainage, bandaging, skin care/wound care, and appropriate exercises.
- Manual Lymphatic Drainage (MLD): Manual lymphatic drainage treatment is a comfortable massage technique performed by a certified therapist that promotes movement to reroute fluid around blocked areas and into healthy lymphatic regions and lymph nodes.
- Compression Bandaging: Compressive bandaging consists of layered short stretch bandages with foam padding under bandage layers. These bandages are used to slow the accumulation of new fluid until maximum drainage has been achieved. At this point, patients transition to custom, pull-on compression garments worn during the day and night to maintain their progress.
- Exercise: Exercises are used to enhance lymphatic drainage and lower the risk of worsening the condition. Exercises may consist of diaphragmatic breathing, active range of motion, strengthening, and stretching.
What to Expect during Lymphedema Therapy?
Initially it is recommended that the patient be seen by the certified lymphedema therapist 4 days per week until the limb is adequately drained. Therapy then tapers to 2-3 days per week until the custom compression garments arrive.