What is a Diabetic Foot Ulcer?
If you are one of the 34.2 million Americans living with diabetes, you could be at risk for a chronic wound known as a diabetic foot ulcer. High blood sugar makes it hard for wounds to heal by reducing the amount of oxygen-rich blood that reaches wounds, especially on lower legs, feet, and toes.
A diabetic foot ulcer is a wound that is usually found on the ball of the foot or the toes. It may start from a cut or scrape or a blister caused by poorly fitting shoes. Additionally, many people living with diabetes have nerve damage in their lower limbs and do not feel pain when an ulcer begins.
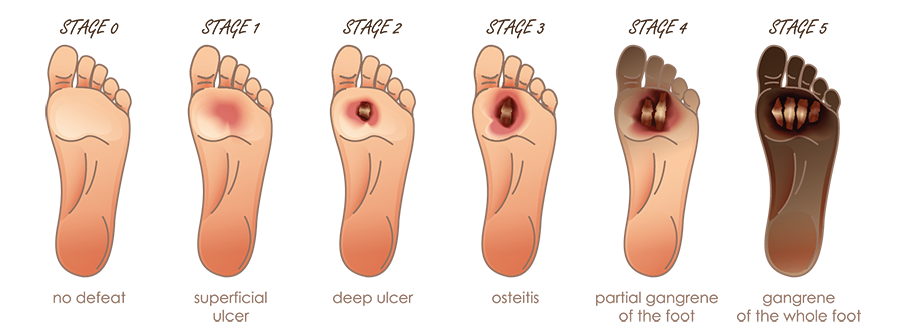
Progression from Ulcer to Amputation
Diabetes-related wounds are a leading cause of limb loss and 10 Americans undergo amputation each hour. Up to 55% of diabetic patients will require amputation on the second leg. Even more alarming, nearly half of those living with an amputation will die within two to three years. Early detection and specialized care from a Wound Care Center® can reduce healing times and amputation risk is reduced by almost half when a multi-specialty wound care team provides care.
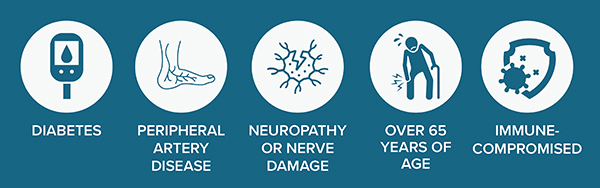
Risk Factors for Diabetic Foot Ulcers
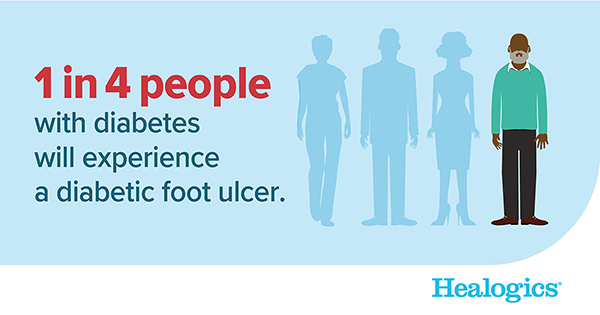
Risk factors for diabetes include age, diet, activity level, obesity, and heredity. Factors that may increase the risks of developing a chronic wound, such as a diabetic foot ulcer, include high blood sugar levels, poor circulation, immune system issues, and nerve damage. Approximately 25% of people living with diabetes will develop a foot ulcer. 85% of diabetes-related amputations started with a foot ulcer.
Several factors can increase the likelihood of developing diabetic foot ulcers, including neuropathy, peripheral arterial disease (PAD), deformities, and Charcot foot.
Neuropathy results from damage to peripheral nerves and often causes weakness, numbness and pain in the hands and feet. Similarly, with PAD, narrowed arteries reduce blood flow to the limbs, causing damage. Charcot’s foot is a deformity that results from nerve damage in the foot or ankle, which may cause injuries to go untreated, leading to the breakdown of joints.
How to Help Prevent Diabetic Foot Ulcers
- Check your feet daily. It works well to incorporate this into your bedtime routine.
- Take your socks off and look your bare feet, heels, ankles, toenails, and between your toes. Look for cuts, scrapes, blisters, red spots, or any other signs of a wound.
- Use a mirror or ask a family member to help.
- Get foot examinations each time you visit your healthcare provider (at least four times a year).
- Wash your feet daily. Dry between your toes well. Do not use powder.
- If your feet become dry, moisturize them, but do not get lotion between your toes.
- Do not go barefoot indoors or outdoors. Wear supportive, properly-fitting shoes and socks.
- Avoid allowing your feet to get too hot or too cold.
- Improve circulation by eating healthier and exercising regularly.
- Stop smoking.
Wound Care Improves Healing and Reduces Amputations
Diabetic foot ulcers have a very high recurrence rate; as many as 40% of people with a healed diabetic foot ulcer will develop a new ulcer within a year. Diabetic foot ulcers can be challenging to heal. Wound Care Centers provide advanced therapies to aid in infection prevention, new tissue growth and successful wound closure. It is important to seek specialized care from a Wound Care Center as soon as an ulcer develops.
Wound care modalities often used to treat diabetic foot ulcers include:
- Debridement is the process of removing dead tissue from wounds. It is necessary for healing because dead tissue hinders the growth of new cells and makes it easier for infection to occur.
- Total contact casting relieves pressure from the wound and is considered the gold standard for treating diabetic foot ulcers.
- Other forms of offloading or taking pressure off the wounded leg or foot, including boots, crutches, or wheelchairs.
- Negative pressure involves placing a vacuum over a dressed wound, which draws the fluid from the body through the wound and stimulates blood flow.
- Hyperbaric oxygen therapy (HBOT) provides patients with 100% oxygen in an enclosed acrylic chamber with higher-than-normal atmospheric pressure, which allows their blood to carry more healing oxygen to the wound.
For more information about the treatment of diabetic foot ulcers, contact Glencoe Regional Health’s Center for Wound Care at 320-864-7040.